Abstract
Background: Pyruvate kinase (PK) deficiency is a rare, hereditary disorder caused by mutations in the PKLR gene encoding the red blood cell PK enzyme (PKR). Defects in PKR lead to chronic hemolytic anemia. Mitapivat (AG-348), a first-in-class, oral, allosteric activator of PKR, is approved by the US Food and Drug Administration for the treatment of hemolytic anemia in adults with PK deficiency. Mitapivat has been shown in the phase 3 ACTIVATE study (NCT03548220) to significantly improve hemoglobin (Hb) and markers of hemolysis and erythropoiesis in patients with PK deficiency who were not regularly transfused. PK deficiency is associated with serious acute and long-term complications, most of which occur as a consequence of chronic ongoing hemolysis and ineffective erythropoiesis. This analysis examines changes in markers of hemolysis and erythropoiesis specifically in patients from ACTIVATE who did not achieve an Hb response as defined in the study protocol.
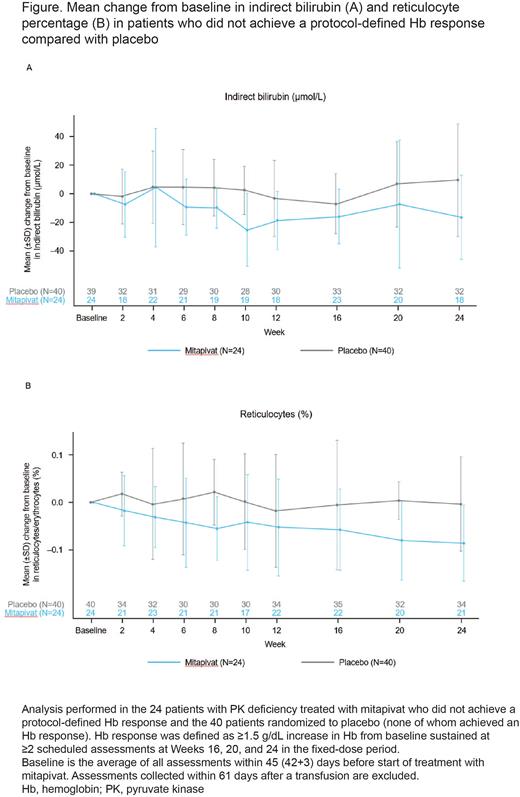
Methods: The randomized, double-blind, placebo-controlled ACTIVATE study consisted of a 12-week dose-optimization period (5/20/50 mg twice daily) and a 12-week fixed-dose period. 80 patients (≥18 years) with a diagnosis of PK deficiency who were not regularly transfused (≤4 transfusion episodes in the prior year; none in the prior 3 months) were randomized 1:1 to receive mitapivat or placebo. The primary endpoint was Hb response, defined as ≥1.5 g/dL increase in Hb from baseline (BL) sustained at ≥2 scheduled assessments at Weeks 16, 20, and 24 in the fixed-dose period. Secondary endpoints included change from BL in Hb concentration, indirect bilirubin, reticulocyte percentage (%), lactate dehydrogenase (LDH), and haptoglobin. The present analysis compared hemolysis and erythropoiesis markers in patients treated with mitapivat who did not achieve the protocol-defined Hb response with those randomized to placebo.
Results: A total of 80 patients were randomized 1:1 to receive mitapivat (N=40) or placebo (N=40). Mean Hb at BL=8.6 g/dL; 16/40 patients treated with mitapivat (40%) and 0/40 (0%) patients who received placebo achieved an Hb response (2-sided, p<0.001). Of the 24 patients treated with mitapivat who did not achieve a protocol-defined Hb response (mean [SD] change from BL in Hb at Weeks 16, 20, and 24: 0.44 g/dL [0.45]), markers of hemolysis and erythropoiesis improved numerically, as shown by a positive average change from BL at Weeks 16, 20, and 24 in indirect bilirubin (Figure A) (BL mean [SD], 98.4 µmol/L [68.4]; mean [SD] change from BL, -12.7 [24.6]); haptoglobin (BL mean [SD], 0.10 g/L [0.13]; mean [SD] change from BL, 0.05 [0.14]); LDH (BL mean [SD], 292.8 U/L [248.7]; mean [SD] change from BL, -27.1 [106.5]); and reticulocyte % (Figure B) (BL mean [SD], 0.48 [0.22]; mean [SD] change from BL, -0.07 [0.07]). For the 40 patients randomized to placebo, none of whom achieved an Hb response, there was minimal or no average improvement from BL at Weeks 16, 20, and 24 in indirect bilirubin (BL mean [SD], 89.1 µmol/L [61.8]; mean [SD] change from BL, 3.0 [20.1]); haptoglobin (BL mean [SD], 0.08 g/L [0.14]; mean [SD] change from BL, 0.01 [0.07]); LDH (BL mean [SD], 260.0 U/L [140.2]; mean [SD] change from BL, -8.7 [76.4]); or reticulocyte % (BL mean [SD], 0.40 [0.22]; mean [SD] change from BL, -0.0004 [0.06]).
Conclusions: Mitapivat directly targets the underlying pathophysiologic defect in PK deficiency by activating PKR. In ACTIVATE, significant improvements in markers of hemolysis and erythropoiesis have been demonstrated for the overall patient population treated with mitapivat. This analysis now shows that directional improvements occur even in patients who did not achieve the clinical trial definition of Hb response. By improving markers of hemolysis and ineffective erythropoiesis, mitapivat is the first oral agent that has the potential to minimize long-term complications in patients with PK deficiency, irrespective of Hb response.
Disclosures
Al-Samkari:Forma: Consultancy; argenx: Consultancy; Novartis: Consultancy; Sobi: Consultancy, Research Funding; Amgen: Research Funding; Rigel: Consultancy; Moderna: Consultancy; Agios: Consultancy, Research Funding; Dova: Consultancy, Research Funding. Grace:Agios Pharmaceuticals: Consultancy, Research Funding; Sanofi: Consultancy; Novartis: Research Funding; Sobi: Membership on an entity's Board of Directors or advisory committees, Research Funding. van Beers:RR Mechatronics: Research Funding; Sobi: Research Funding; Sanofi: Consultancy; Novartis: Research Funding; Pfizer: Research Funding; Agios Pharmaceuticals, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Global Blood Therapeutics: Consultancy. Tai:Agios: Current Employment, Other: Stockholder. Morales-Arias:Agios: Current Employment, Other: Stockholder. Beynon:Agios: Current Employment, Other: Stockholder. Glenthøj:Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Saniona: Research Funding; Sanofi: Research Funding; bluebird bio: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy; Pharmacosmos: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal